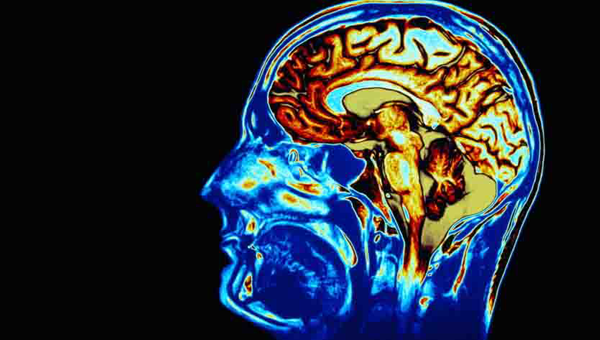
As a non-invasive “operation”, CyberKnife has proven to be an effective alternative to surgery or conventional radiation for treating vascular abnormalities, tumors, functional disorders, and cancers with sub-millimeter accuracy. CyberKnife gives renewed hope and the possibility of a better quality of life, especially for patients with tumors previously diagnosed as inoperable, and for those who have already received the maximum amount of radiation through other treatment methods.
As a non-invasive “operation”, CyberKnife has proven to be an effective alternative to surgery or conventional radiation for treating vascular abnormalities, tumors, functional disorders, and cancers with sub-millimeter accuracy. CyberKnife gives renewed hope and the possibility of a better quality of life, especially for patients with tumors previously diagnosed as inoperable, and for those who have already received the maximum amount of radiation through other treatment methods.The CyberKnife uses non-invasive image-guided localization that is more convenient and less traumatic than other systems using the standard invasive stereotactic headframe (a rigid metal frame fixed to a patient’s skull for head immobilization and target localization). CyberKnife also uses an advanced, lightweight linear accelerator (LINAC), a device used to produce a high dose of radiation.
In addition, CyberKnife also has a robotic delivery system that not only provides the flexibility to reach areas of the body unreachable by other systems, but is also instrumental in precisely aiming the device.
The robotic delivery system integrates motion-tracking software, called the Synchrony System, with the robotics, making it accurate enough to even hit a moving target. As a patient breathes or moves slightly during treatment, the robot detects the motion and compensates in ‘real time’, ensuring that the radiation is accurately hitting the target (tumor) throughout treatment.
CyberKnife can strike the tumor with a high dose of radiation from over 1200 different angles. This pinpoint accuracy allows malignant or benign tumors to be obliterated without damaging critical healthy tissue.
How is CyberKnife Different ?
Standard stereotactic radiosurgery techniques rely on a rigid frame fixed to the patient's skull for head immobilization. There are other systems for extra-cranial Stereotactic Radiation. These systems are most often uncomfortable. If the target moves with the breathing of the patient, they often require breath holding techniques, which may be difficult for some patients. Frame-based systems mean there is a limit to the number of angles the radiation can be delivered through.
The CyberKnife System offers maneuverability and versatility that other systems cannot offer, therefore now making it possible to treat tumours anywhere in the body, especially the brain, spine, liver, lung, pancreas and prostate. The combination of image guidance with the help of X-ray cameras and the very latest computer technology ensures that the CyberKnife® System is able to overcome the limitations of older frame-based radiosurgery systems, such as the Gamma Knife and LINAC based X-Knife.
treatment to the tumor alone,
sparing surrounding healthy tissue.
|
What
can the CyberKnife treat?
The CyberKnife Robotic Radiosurgery
System is a non-invasive alternative to surgery for the treatment of both
cancerous and non-cancerous tumors anywhere in the body, including the
prostate, lung, brain, spine, liver, pancreas and kidney. The treatment - which
delivers high doses of radiation to tumors with extreme accuracy - offers new
hope to patients who have inoperable or surgically complex tumors, or who may
be looking for a non-surgical option.
What
is the treatment course?
CyberKnife treatment is performed on
an outpatient basis. The patient receives an initial consultation with the
radiation oncologist and surgeon. A CT scan (3-D X-ray) is obtained. The 3-D
image obtained is used by the physicians, physicists and team to create a treatment
plan.
The patient will return for the
one-hour treatment within a few days after the consultation.
The number
of treatments will vary depending on tumor size, location and shape, but the number of treatments is usually
between one and four.
- Better quality of life during and after treatment
- Head frames not used as with other stereotactic
radiosurgery programs
- Performed on an outpatient basis
- Less pain
- No incisions
- Risk is minimized to healthy tissue surrounding
tumor/lesions
- Fewer visits to the hospital
- Short recovery period
- Treatment is available for tumors considered inoperable
by other surgery and stereotactic radiosurgery methods
- Lower risk of complications when compared to other
treatment options
- Lower risk of infections
- Lower risk of hemorrhage/severe blood loss
- Lower risk of hearing loss
- Lower risk to alteration in feeling of extremities
Please
scan and email your medical reports to us at care@medworldindia.com and we
shall get you a Free Medical Opinion from India’s Best Doctors.
Call Us : +91-9811058159
Mail Us : care@medworldindia.com



.jpg)




.jpg)